Midwife Goldilocks And Her Measuring Tape
Sep 16, 2023
Once upon a time midwife Goldilocks was given a measuring tape and she was told that this would be how she could tell which babies were too big, which babies were too small and which babies were just the right size.
For a long time Goldilocks did exactly what she was asked to do even though she felt she shouldn't. One day, she got brave enough to give the tape back and she skipped into the sunset.
...or something like that...
In my recent blog post ‘About Birth And Whiskey’ I asked the question of how midwives had ended up with a measuring tape and customised growth chart to assess a baby’s growth. The measuring tape is one of the reasons I finally let go of my registration, I loathe them with a passion. This week I want to elaborate a bit on why I take so much issue with them.
And it’s not only me, many former colleagues of mine who truly value holistic and authentic midwifery care also despise the practice of plotting measurements on a computer generated graph apparently reflective of what size of a baby this particular woman in front of them should grow.
This screening tool is so sensitive at the time of your first measurement that a referral for a scan later down the line is almost inevitable. At 26 weeks the difference between a 'small baby' on the 10th centile and a 'big' baby on the 90th centile is defined by 6 millimetres across a pregnant belly. Your midwife has to identify the tip of your pubic bone and she has to decide the highest part of your baby bump. Then she measures and plots.
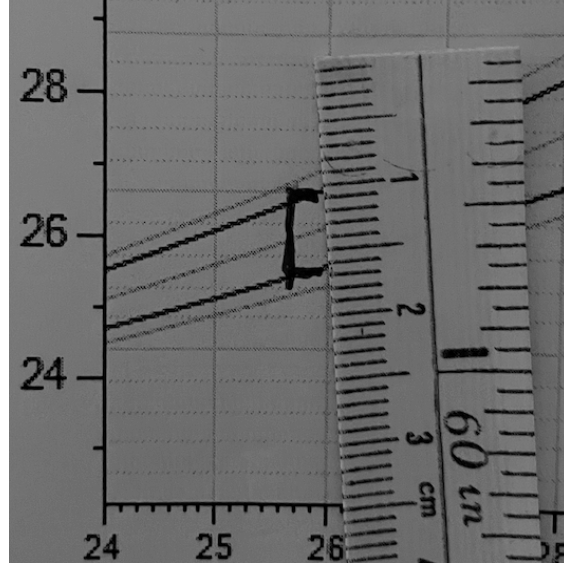
She measures repeatedly at least two weeks apart and whether you must be referred for a scan or not depends on the 'curve' of the plotted measurements.
Here's a graph that shows growth along the same centile:
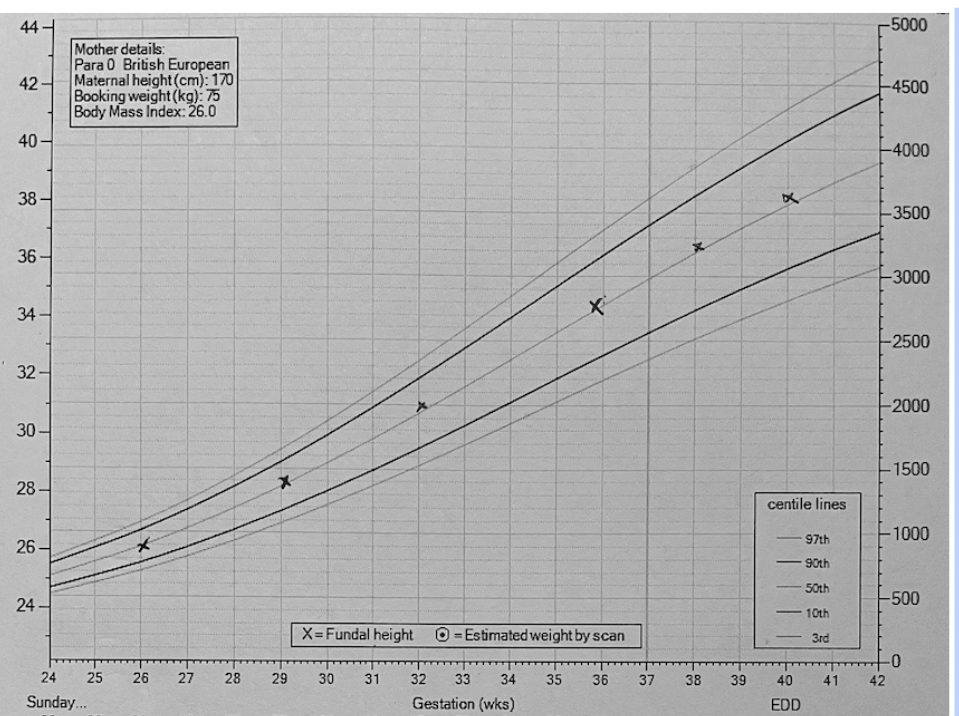
Any 'crossing centiles' warrants referral for an ultrasound scan. Again, a few millimetres across a round pregnant belly could make the difference. It just makes no sense. It has to be sensitive to over referrals and if scans were reliable in predicting a baby's size, and if a baby's size beyond the situation of having a growth restricted baby actually mattered, then that would be swell. But they are not; and it doesn't!
When I looked more closely at evidence to reference in my book ‘7 secrets every pregnant woman needs to hear before giving birth’, my suspicions were confirmed. The tape is nonsense! I found a study published in 2020 in a professional journal called Ultrasound in Obstetrics and Gynaecology that looked at 11 million births. It found no conclusive evidence to suggest that the customised growth charts improve babies’ outcomes.
The tapes and growth charts need to be considered in the wider context. First of all, they are used on 'low risk' women. These are the women least likely to develop pregnancy complications. These are the women midwives are 'allowed' to look after within the obstetric model. Supported in authentic midwifery models these are women who could have a less than 2% chance of needing a caesarean section! Yes, you read that right. There are places in the world where healthy women are this unlikely to need any kind of medical assistance and they give birth to healthy babies. Check out 'The Farm' midwifery centre for one example of this. By measuring their bellies with this highly unreliable method we expose a large number of these healthy women and babies to further interventions that they don't need. Considering the limitations of ultrasound scans and the risk of induction of labour and caesarean sections, this is objectively harming 'low risk' women within mainstream maternty care.
Knowing this bigger picture and knowing that none of it was aligned with my own values was tough. During my last few shifts as a midwife in the antenatal clinic I felt a wave of nausea every time I unfolded one of the paper tapes to run it over someone’s pregnant belly; my body giving me a clear message to get myself outta there.
The vast majority of concerns that arise in industrialised midwifery and obstetric practice are imagined by the care providers in response to interpreting routine screening procedures. Those procedures may be based on no evidence of benefit whatsoever and 'positive' findings may in essence be entirely meaningless and benign but they take you on the gravy train to a surgical birth. And even though we don't see the NHS as an industry because 'free at point of contact' and all that jazz, make no mistake. The NHS is part of the medical industrial complex. In the end policy is reflective of who holds most power and your healthcare is not 'free', just look at your paycheck.
Last week, Erin from Better Birth UK released an Instagram post saying ‘When a hospital’s induction rate is almost 61%, the system we’re birthing in is broken…not our bodies or ability to birth unassisted’. The hospital she is referring to is here, in Northern Ireland, and they were sporting a 40%-50% overall caesarean section rate in December 2022 - I heard on the grapevine that early this year the C/S rate there was over 60%. Inductions of labour lead to more caesarean sections, period! Erin is right! This is not an indicator that 61% of babies or mums are in trouble, it indicates a systemic problem. Fear based defensive practice is the issue here, not women and their babies.
Inductions happen because midwives and doctors are not prepared to leave things alone unless they are ‘just right’ as defined by poorly evidenced guidelines. There are Goldilocks everywhere!
Baby too big? - No problem, let’s do an induction.
Too small? - Same solution.
Mama too old? Don’t wait until 40 weeks.
Your pregnancy is lasting too long? - Guess what? Best to induce at 41 weeks.
You’ve got gestational diabetes? - Sure, let’s induce.
Blood pressure is a little too high? - You guessed it.
That’s how you end up with an induction of labour rate of 61% and that doesn’t even count the women who had membrane sweeps or women who had their labours augmented (where a drip gets put up in a spontaneous labour to make more contractions). Very few women get through labour without ‘a little help’.
But why is this such a big deal?
Not everyone is mother earth and women don't mind!
Believe it or not, how an individual woman chooses to have her baby is totally irrelevant to me.
I will support her.
I will help her find a way to make her journey meaningful in her context.
I will cheer for her.
I will admire her baby and support her in the fragile early days of parenthood.
I will listen to her and try to really hear her.
When she needs a shoulder to cry on I will be there.
I have done all this for many years. An individual woman will only get support and love from me.
It's because of this love for all women that I am not prepared to gaslight any of them. Women come to me all the time having felt railroaded into decisions that led them so far away from their dream birth that they are now hurting. Often birth starts to derail after someone did something to them. That tape measurement that led to the scan that led to the estimated big baby that led to the sweep that led to the induction of labour that led to the drip that led to the continuous monitoring that led to the concern about the baby's heart beat that led to the caesarean that led to the difficult breastfeeding that led to despair that led to postnatal depression. I will not pretend that that's okay. I will not be one of those people who tell you that 'a healthy baby is all that counts' or 'you want your baby to be safe, don't you?'. I will not pretend that this is okay and I will never tell you that the way things are is the way that they have to be for your and your baby's safety. Far from it!
The only thing I know to do is tell the truth about what I have learned over the years and that is that midwifery as we know it today is based on viewing pregnancy through a medical lens and the measuring tape is one of the expressions of this and it is without a doubt one of the reasons the induction of labour rate is so high.
You might think that if an induction of labour saves only one baby then it is worth the trauma and women can get over it, right?
No, medical care only truly benefits a handful of women and babies and thank goodness it's there when needed. In the majority of cases your midwives and doctors save you from problems they first created themselves by interfering, not from an intrinsic problem. And, as it turns out induction of labour does not prevent stillbirth in 'low risk' women, so you are trading all the disadvantages an induction brings for you for no benefit for your baby. To the contrary, your baby will also be at a disadvantage as a result of an induction of labour. And that disadvantage lasts to adolescence (possibly a lifetime, but so far we only have data for the first 16 years of life).
Check this out:
The Australian midwifery researcher Dr Hanna Dahlen published a study in 2021 that summarised findings from almost half a million women giving birth between 37 and 41+6 weeks. It was conducted between 2001 and 2016 and it is the only study that followed up children into adolescence. It found that while induction rates have tripled between 2001 and 2016 in New South Wales, the stillbirth rate has not reduced. The study shows that statistically speaking, induction of labour causes more problems in women and their infants than spontaneous onset of labour does.
The study found the following disadvantages of an induction of labour for women:
Increase of epidural or spinal analgesia use.
Higher chance of having a caesarean section.
Higher chance of an instrumental birth.
Higher chance of having an episiotomy.
Higher chance of having a postpartum haemorrhage.
The disadvantages for the baby and up until the age of 16 are:
Higher rates of birth asphyxia (low oxygen during labour).
Higher rates of resuscitation at birth.
Higher rates of birth injuries.
Higher rates of respiratory issues.
Higher rates of hospital admissions for infection.
(Dahlen, et al., 2021)
When I first was taught how to palpate a woman’s abdomen, there was an emphasis placed on the amount of information one can glean by simply being with her. Without ever touching her you can learn about her state of emotional, physical and perhaps even spiritual wellbeing by listening and by looking.
Does she seem full of energy or is she tired?
What colour is her skin today? Does she look pale or is her face glowing?
Can you tell if she seems well hydrated and well nourished or does she look weak and dry?
Is her voice full of confidence or does she seem hesitant and unsure?
What kinds of things is she saying, do her words imply confidence and happiness?
Looking at her belly could you guess the phase of pregnancy she is in? Does it look uncomfortably taut and shiny or can you see the outline of the baby? Are there any scars? What shape is her belly?
An abdominal palpation can only ever be meaningful in the context of the big picture and midwives know this! To me, the job of a midwife in its true sense seems fairly straightforward. A midwife needs to know pregnancy physiology and understand how to support its unfolding. She needs to help women find ways to nourish their bodies with wholesome foods and a complete diet with healthy sources of fats and proteins. The midwife is there to support her clients’ emotions as they are expanding to welcome new life, she listens and she sees; she understands that the most likely outcome by far is that a pregnancy will result in an uncomplicated birth and a healthy baby. Because of the relationship the midwife has with the mamababy, she can pick up on those rare instances when a palpation might reveal that something is truly amiss. Too much fluid, too little fluid or a tiny baby can be spotted in this way. Those truly are reasons to get a doctor involved because they might indicate a problem. The woman might already know herself that something isn't right and she needs her midwife to support her in knowing what to do next. If we support women in those ways or if the woman finds a way to support herself in those ways the likelihood of loosing a baby is slim. It's not impossible but it is highly unlikely, and if it happens it is important for the woman to be held in knowing that it is not her fault, never. That is also a midwife's job.
Instinct, intuition and true compassionate human connection suffer when our decisions are based purely on numbers and guidelines. The number on the tape measure can easily distract from the visceral messages you are getting in a woman's presence. Midwives still say words to women like 'trust your body' which is amazing but then in the same breath we say '...but let's just check with the scanner to see if baby is really okay'. It's a contradiction. Do we trust ourselves or do we trust routine interventions that have repeatedly been proven unreliable in predicting any kind of outcome? Industrialisation and technology can never replace human relationships.
Let's find a way back to seeing the value in authentic midwifery.
References:
UK stillbirth trends in over 11 million births provide no evidence to support effectiveness of Growth Assessment Protocol program - GAP
https://obgyn.onlinelibrary.wiley.com/doi/10.1002/uog.21999
Dahlen, et al (2021). Intrapartum interventions and outcomes for women and children following induction of labour at term in uncomplicated pregnancies: a 16-year population-based linked data study. BMJ Open. 2021;11(6):e047040. Accessed via: https://pubmed.ncbi.nlm.nih.gov/34059509/

