In Search Of My Tribe
Aug 26, 2023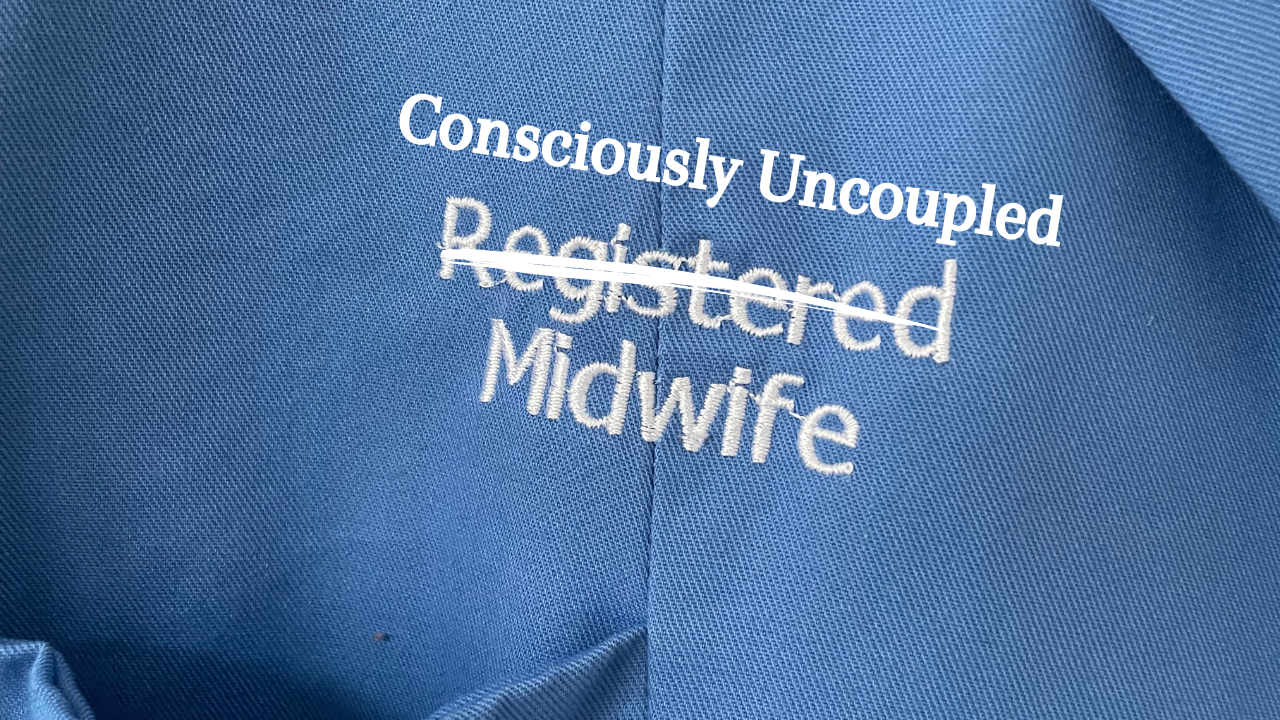
That yearning I felt after witnessing my first birth would stay with me through my first labour ward placement. I remember torturing my poor mentor with questions she just couldn’t answer. What if we had left it alone? Do you think she just needed more time? Did she really need that induction of labour? Ultimately nobody can answer what would have been, we don’t have crystal balls. We continue to learn from our experiences and those are built on the shaky foundations and poorly evidenced guidelines of obstetric practice.
My mentor was still a great teacher. I learned lots from her about how to be a labour ward midwife and I wanted to know what she knew. She was so confident and experienced. She didn’t think twice about looking after a twin mama in labour or looking after someone with pre-eclampsia. She had eyes like a hawk and a heart of gold and her decision making was solid, no hesitation. I admired her in so many ways. She’s retired now, but there are still countless midwives like her on labour wards everywhere and we need them. We need them because sometimes birth becomes complicated and we need them to care for those women who want to use the tools available in modern labour care.
I think one of the reasons my mentor was so good at her job as a labour ward midwife was that she was very accepting of the routine care pathways. She didn’t feel a need to question how those pathways came to be, the induction of labour rate or the caesarean section rate. One shift, after wheeling a woman out of theatre I asked my mentor if she thought that the induction of labour and the epidural had contributed to the caesarean. She shrugged and said ‘square peg, round hole, baby just didn’t fit’.
For her it was that simple!
In many ways I wished that I could see it that way, I think it might be an easier gig if you can. The clinical skillset of a midwife is impressive. Getting good at all of the skills a midwife needs requires a lot of practice. Experience is hard earned and continued learning requires resilience and it happens in fast paced environments. It's understandable that midwives want to focus on developing their clinical skills rather than challenging the narrative.
As a student midwife and to this day I have wondered about the impact of the journey to the labour ward, the messaging in pregnancy. Your baby is too big, too small, too late; you are too thin, too heavy, too selfish. What does hearing that do? Do those suggestions in themselves dampen a woman’s belief in her ability to give birth to her baby, and, importantly, does a dampened belief inhibit the subtle and delicate processes of our physiology? Are those processes protective in themselves? What do those suggestions do to the care providers' trust in the process? How much harm does fear of birth do to our collective consciousness and how does our readiness to move to surgical birth undermine the safety of potential future siblings in the family of this mama/baby right now?
I have always felt that we were doing women wrong by pushing the idea that medical technology is superior to their physiology and their own intuition and instinct. How can anyone know better than the parents themselves? And how was it that, at midnight on the tenth day past 40 weeks, things changed so drastically that we had to ‘bring you in for induction’? I wanted those conversations and I was seeking out opportunities to have them. Through those conversations I found many midwives who will advocate for women who want a physiological birth. I have witnessed midwives who will support women who decline inductions of labour or routine prophylactic medicines such as Anti-D or Vitamin K for their babies. Parents are the people who are most invested in their children’s health, period, and I am lucky to know midwives who see it that way, midwives who know that parents need their unconditional support regardless of whether they agree or disagree with parents choices and regardless of what happens in the end (if you haven't already, I highly recommend reading Dr Sara Wickham’s books to provide perspective to you as a parent or practitioner).
Many of those conversations happened during my annual community placements. My community mentor runs like a thread through my training. Our relationship grew as I grew into a fully fledged midwife. We spent a lot of time together driving from home to home, talking. I introduced her to some of my ideas and she spoke of her years of experience in the community. She got me and she got why women wanted to birth at home and she supported them. She had seen many homebirths and she was able to offer me perspective on my ways of thinking - I needed that. At the time, I believed that if we tried hard enough, every caesarean and every instrumental birth could be avoided and of course that’s naive and total nonsense. To me every single intervention equalled a negative birth experience and every physiological birth was by definition blissful and of course I was projecting. I held some other beliefs that clearly revealed my bias towards trusting women over medicine. Over time I discovered those biases that are held by those practitioners who trust medicine over physiology. Neither approach gets it right every time and the art lies in striking a balance. The medical model's pipe dream is that we can prevent every tragedy and that's unrealistic and it comes at a price but the holistic model has its own blind spots. There will always be women who need a team of doctors to help them give birth to their babies. There is merit in honouring and trusting birth physiology AND modern medicine can save lives.
On August 6th, 2006 I went to a homebirth support group meeting. I met a midwife from the first alongside midwife led unit in Northern Ireland and an independent midwife from the United States of America. I didn’t think to note in my diary which of the United States she was from, only that her name was Kim. She was the second independent midwife I ever met. The other was a midwife in Germany who we worked with in the aromatherapy shop I jobbed in as a young woman. Kim was the first person to get me thinking about pelvic and spinal alignment and its relation to childbirth. I noted ‘find out: chiropractic technique to position foetus for birth’. Kim must have mentioned it and I forgot the name of it (it’s Webster’s). Talking to Kim blew my mind that evening. This encounter sent me on the path to combining my work as aromatherapist and body worker with my passion for midwifery and childbirth, the path I am still walking today.
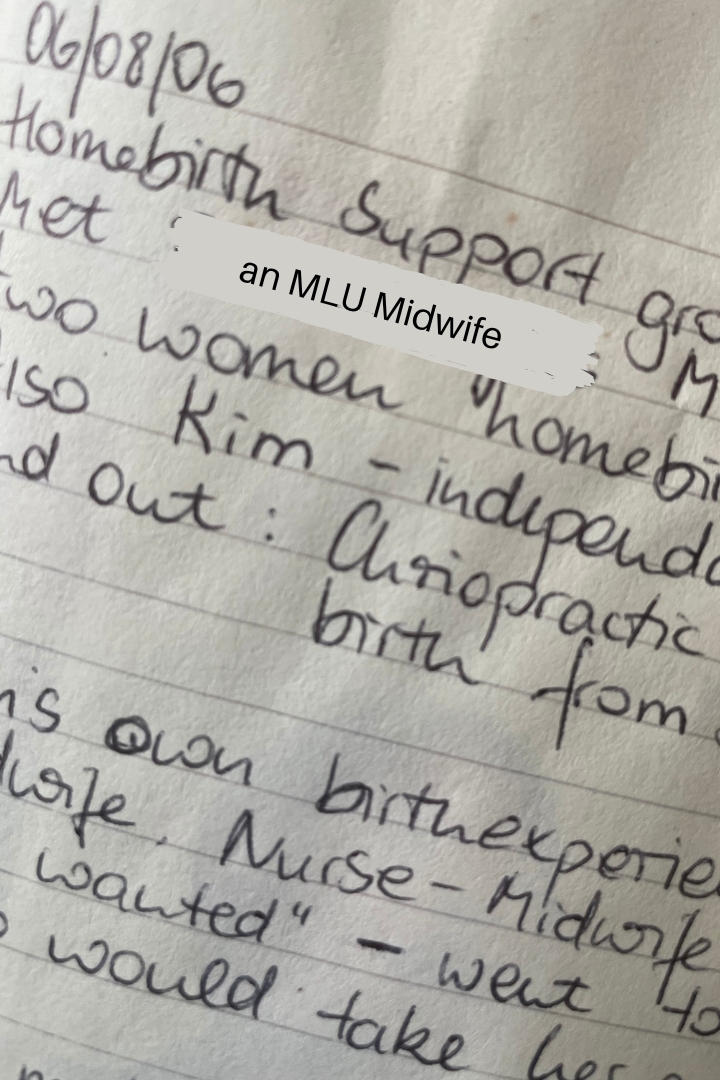
I volunteered to drive Kim to where she was staying in North Belfast and got her all to myself on a twenty minute car ride. She told me her own birth experience had made her want to be a midwife and that she trained as a ‘nurse-midwife’. Nurse midwifery is one of the pathways into midwifery in the USA where there is a clear distinction between people who see midwifery the way I do and those who feel more rooted in the medical paradigm. Kim felt nurse midwifery was close but not quite what she wanted from her work with women and so she enrolled for an apprenticeship with an independent midwife. We didn’t stay in touch so I don’t know what Kim is up to now, but at the time she loved her way of working and I could relate to her so much. That feeling of being close, but not quite there…I knew it well. Who could I apprentice with in Northern Ireland? Who worked like this? I hadn’t found them yet, but I would try!
Back at uni we were going to meet two midwives from the caseload midwifery team in the Belfast Trust. When the two of them came to speak to us I totally loved them! That team saw women right through from start to finish. Six midwives working in teams of two. The women really got a chance of forming a relationship with their midwives and then one of the two named midwives would be there for the birth of the baby. Now we were talking. This was exactly what I wanted. Those midwives spoke about how much they learned from being with women all the way through, this way of working gave them direct feedback about their own practice and they felt it expanded their learning immensely. There it was. I knew instantly that I would try to land myself right in that team as soon as I possibly could. First I would have to qualify and then I would have to get some experience on rotation. I gave myself about five years. There was only one problem: Every single one of the six midwives loved their job and there was no intention to expand the team. I would have to keep a close eye and pounce at the first opportunity.
To be continued...

